STEM CELLS MAY MAKE TRANSPLANTS HISTORY
Gene Therapy Is Being Used To Regenerate Parts Of Organs Like Liver And Kidney
V Ayyappan | TNN
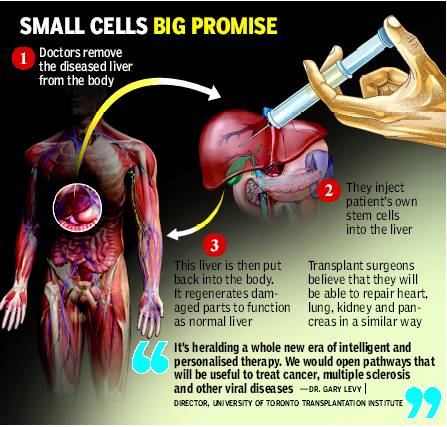
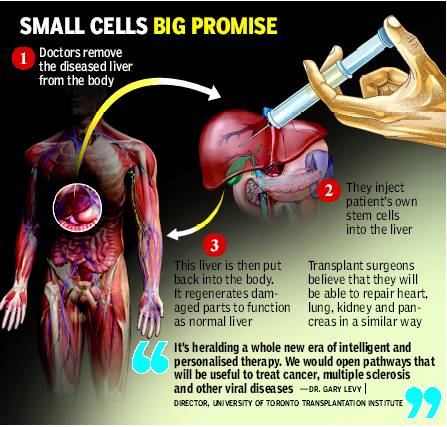
In the near future, doctors will be able to take a liver out, repair it and put it back even as the patient is on the operating table. This could end the harrowing wait of end-stage liver failure patients for donor organs, as a scientific project by a team in the University of Toronto Transplantation Institute promises. India, where several hospitals do stem cell therapy, may be able to utilise the breakthrough to save its increasing number of liver patients.
The big promise comes from tiny stem cells, said Dr Gary Levy, director, University of Toronto Transplantation Institute, who was in the city for a conference on regenerative medicine. “Growing patches for a lung, kidney or heart, from a patient’s own cells may soon be possible. These patches can be used to replace ailing organs,” he said.
University of Toronto Transplantation Institute is already using gene therapy to regenerate parts of liver by injecting genes as soon as they are harvested. “We are planning to do the same with heart and kidney. Studies have found that human donor lung can be repaired to a large extent by delivering a gene, 1010, to increase oxygen capacity. International studies are on to confirm this,” said Dr Levy. “We are able to service only 40% of patients because of shortage of good donor organs. Increasingly, people under 50 need multiorgan transplants. About 10 million people die of organ failure across the world every year,” Dr Levy said.
The experiment in the university began some years ago, when doctors were trying to repair organs that came as donations from brain dead patients. Brain death is an irreversible condition when the brain loses control over other vital organs. In more than 90% of the cases a head injury due to accident causes the condition.
Such patients are considered clinically dead, but their organs can be used to replace ailing ones in patients whose organs have failed. With the number of patients with heart, lung, kidney, liver and pancreas failure growing, the demand for organs have been increasing globally. But transplant surgeons are forced to give up some organs as they aren’t fit for transplant. “If we repair them, we could minimize wastage,” Levy said. Another challenge is to ensure that once transplanted, the new organ is not rejected by the body.
During the experiment, doctors stumbled upon another possibility: repairing patient’s own organ on the operation table. The transplantation institute at the University of Toronto, he said, was using stem cell therapy to regenerate parts of liver and lungs.
For instance, when a lung failure patient is on the operation table, doctors stop the lungs and connect the patient to a machine that ‘breathes’ for him. Meanwhile, doctors can take out the lungs and inject stem cells that can improve their capacity to absorb oxygen. In many cases, patients have been able to avoid or delay transplants, he said. The institute is planning to work on heart and kidney. Similar treatments could be used to remove fat from liver. Excess fat in the liver can cause the organ to fail.
Many people undergoing transplants are now being given immunosuppressive drugs. Regenerative medicine can be used to reduce their requirement, Dr Levy said. “It’s heralding a whole new era of intelligent and personalised therapy. We can re-educate the immune system. If we manage to do that with organ transplant, we would open pathways that will be useful to treat cancer, multiple sclerosis and other viral diseases,” he said.